Abstract
Introduction: Total Body Irradiation (TBI) conditioning regimens are considered standard of care for pediatric hematopoietic cell transplant (HCT) recipients. However, TBI has many long-term effects, so avoiding it in young HCT recipients is critical. Fludarabine is frequently used in combination with other chemotherapeutic agents like busulfan and/or thiotepa in non-TBI based conditioning regimens. While multi-drug conditioning aims to avoid TBI-related late-effects, little is known about the effect of variations in genes that metabolize these drugs (pharmacogenomics/PGx) on clinical outcomes including engraftment, relapse, and acute drug-related toxicities. In this study, we investigated the pharmacogenomic effects on HCT outcomes such as event-free outcomes and re-transplantation outcomes, as well as fludarabine's pharmacokinetics (PK).
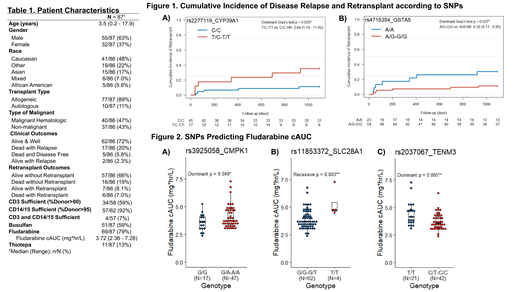
Methods: This ongoing study included pediatric patients from a nationwide multi-center study who received fludarabine in combination with other agents as busulfan and thiotepa. From literature searches and PharmGKB databases, we selected 70 SNPs in 30 candidate pharmacological genes for these drug pathways. SNPs with a minor allele frequency of 10% were further selected for analysis with different endpoints such as: 1) Cumulative incidence with disease relapse with re-transplantation (using Gray's methods, controlling for competing risks); 2) fludarabine PK with cumulative area under the curve (cAUC); 3) 1-month-post-transplant chimerism levels defined as sufficient (CD3 ≥80% and CD14/15 ≥95% chimerism) and insufficient (CD3 <80% and CD14/15 <95% chimerism); and 4) event-free outcomes (comparing patients alive and well vs. others) OR alive re-transplantation outcomes (alive with vs. without re-transplantation). SNPs with an association p-value <0.05 were considered significant using generalized linear models from the SNPassoc R package.
Results: Total of 87 patients included in the analysis had a median age of 3.5 (0.2 - 17.9) years, 63% were male, 48% were Caucasian, 85% had received allogenic HCT, and 43% had malignant hematologic disease (Table 1). For SNP rs2277119 in CYP39A1, presence of T allele was associated with greater cumulative incidence of re-transplantation (TC-TT vs. CC genotype: HR=3.64 (95% CI=1.14-11.62), p=0.02, Figure 1A); and SNP rs4715354 in GSTA5, presence of G allele was associated with lower cumulative incidence of re-transplantation (AG-GG vs. AA: HR=0.32 (95% CI=0.11-0.95), p=0.037, Figure 1B). In 79% of patients with available fludarabine cAUC (median of 3.72 mg•hr/L), we evaluated fludarabine pathway gene SNPs for association with cAUC. Within SNPs rs3925058 in CMPK1 and rs11853372 in the uptake transporter SLC28A1, presence of variant allele was associated with higher fludarabine cAUC (rs3925058: GA-AA vs. GG, p=0.049, Figure 2A, and rs11853372 GG-GT vs. TT, p=0.003, Figure 2B); and for a 3'-UTR SNP rs2037067 in TENM3/DCTD, the variant allele was associated with lower fludarabine cAUC levels (CT-CC vs. TT, p=0.005, Figure 2C). In an exploratory analysis with event-free outcomes, patients with variant allele for SNPs rs9937 in RRM1, rs2072671 in CDA, rs324148 in SLC29A1, and rs7533657 in CTPS1 had higher odds of having an event compared to patients with the reference allele; while rs11577910 in CTPS1 had a better outcome with presence of variant allele. With respect to patient's status being alive with re-transplantation outcomes, variants SNPs with rs507964 in SLC29A1, rs4244285 in CYP2C19, rs1021737 in CTH, rs1561876 in STIM1, and rs1130609 in RRM2 have high odds of re-transplantation. At 1-month follow-up, variant SNP rs12144160 in CTPS1 was associated with sufficient chimerism in CD3 and CD14/15.
Conclusions: In this study, we have identified a number of SNPs that predict interpatient variability in clinical outcomes and fludarabine levels in pediatric HCT recipients. Results so far showed potential to predict outcomes and develop strategies that will consider pharmacogenomics when determining fludarabine doses in pediatric HCT recipients. Our ongoing study is focused on establishing and validating the pharmacogenetic markers predictive of pharmacokinetics of busulfan, fludarabine and thiotepa and clinical outcomes in pediatric HCT recipients.
Acknowledgements: This study was supported by Florida Department of Health - Live Like Bella Discovery Award (9LA04).
No relevant conflicts of interest to declare.